Key Takeaways
- AI delivers data-driven objectivity in ADHD assessment: Automated tools now analyze behavioral, neurocognitive, and real-world data streams, providing objective insights that help minimize subjectivity and reduce human error often seen in traditional diagnosis.
- Machine learning models outperform classic checklists in diagnostic accuracy: Early research demonstrates that AI-enabled ADHD screening, especially when combined with neuroimaging or large-scale behavioral datasets, often surpasses the consistency and speed of standard rating scales and interviews.
- Integration, not replacement, amplifies clinical expertise: The most effective AI systems are designed to supplement skilled clinicians, supporting nuanced case analysis and guiding further evaluation steps without undermining professional judgment.
- Ethics and privacy demand rigorous attention: AI-driven ADHD assessment introduces critical concerns regarding sensitive data use, transparency, informed consent, and risks of algorithmic bias. Robust safeguards are essential before these technologies see mainstream adoption.
- Hybrid models blend high-tech and human touch: The synthesis of AI predictions with clinical interviews and traditional assessment tools leads to more reliable, individualized diagnoses, preserving the empathy and contextual understanding that only human practitioners provide.
- Virtual reality and wearables expand real-world symptom capture: The latest AI solutions utilize VR platforms and wearable devices for dynamic, ecologically valid assessment that can measure attention and impulse control in realistic, everyday settings.
- AI’s hidden superpower: personalizing treatment and continuous monitoring: Beyond diagnosis, AI models promise targeted intervention planning and real-time progress tracking, opening pathways for adaptive, highly personalized ADHD care.
- Future innovation depends on clinical validation and ethical deployment: Moving from promising pilot studies to real-world clinical practice will require thorough validation, wildly diverse training data, and unwavering commitment to ethical best practices.
By unpacking both recent breakthroughs and persistent roadblocks, these takeaways illustrate how AI has the potential to redefine not just how ADHD is described on paper, but how it is navigated in the real lives of neurodivergent individuals. Dive into the article to discover where technology and human-centered care intersect. See how this intersection can forge a smarter, fairer future for neurodevelopmental assessment.
Introduction
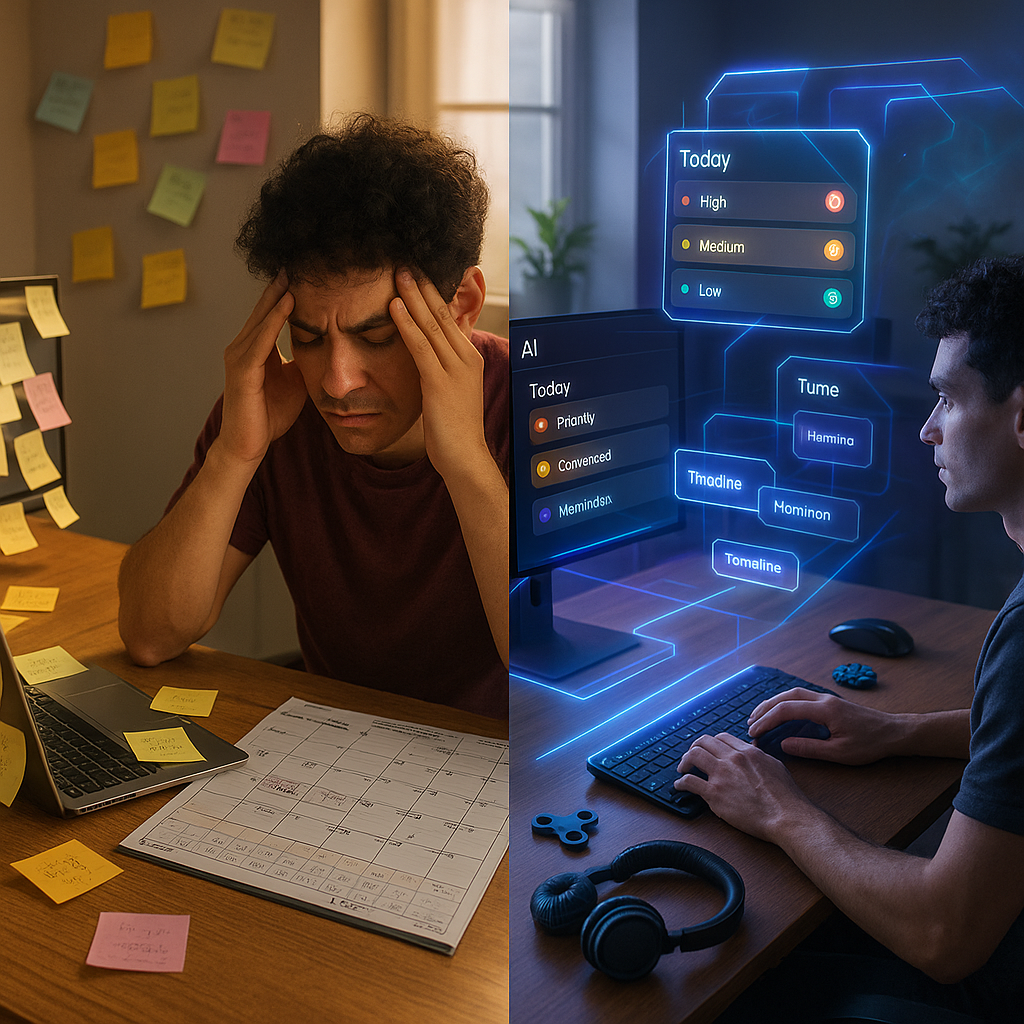
Obtaining an ADHD diagnosis has rarely been straightforward. The process too often relies on subjective checklists, human bias, and the unique complexities of neurodivergent minds, obscuring the clinical picture. Artificial intelligence is now beginning to rewrite this narrative, offering unprecedented objectivity and efficiency in ADHD assessment through sophisticated data analysis and machine learning.
AI can analyze behavioral data in real time and support nuanced clinical decision-making, marking a new era for both practitioners and patients. Yet, with these advancements, issues such as privacy, ethics, and the enduring importance of clinical expertise require just as much attention.
In the following sections, we will explore how AI is transforming ADHD assessment, examining its current capabilities, real-world limitations, and the ethical challenges that will shape the future of diagnosis for neurodivergent individuals worldwide.
The Evolution of AI in ADHD Assessment
From Subjective to Data-Driven Approaches
The diagnosis of Attention Deficit Hyperactivity Disorder (ADHD) has long hinged on clinical judgment, drawn from behavioral observations, patient interviews, and standardized rating scales. While indispensable, these methods have been plagued by challenges like diagnostic inconsistency, clinician bias, and the lack of objective markers to measure attention, hyperactivity, and impulsivity.
AI’s integration into ADHD assessment began in the early 2000s with basic pattern recognition algorithms analyzing data from continuous performance tests (CPTs). These early tools marked the initial shift toward quantifiable, objective measurements capable of supplementing traditional clinical insights.
By 2010, more sophisticated machine learning algorithms emerged, capable of analyzing multiple data streams, including:
- Computerized testing outcomes
- Actigraphy-captured movement patterns
- Eye-tracking measurements
- Speech and language features
The most notable breakthrough occurred between 2015 and 2020, as deep learning architectures demonstrated the ability to detect highly nuanced behavioral patterns that were previously imperceptible to even the most experienced clinicians. For example, a 2019 study by Duda et al. found that convolutional neural networks could identify ADHD-specific attentional patterns with 91% accuracy using only eye movement data during standardized tasks. Traditional assessment methods generally yielded a lower 70-80% diagnostic accuracy.
Current Technologies in Clinical Practice
Today’s ADHD assessment landscape incorporates several AI-powered technologies, each providing unique value:
1. Behavioral Analysis Systems
These advanced platforms capture and analyze dozens of micro-behaviors during standardized tasks. The QbTest system, as one example, fuses computerized performance metrics with motion tracking to quantify ADHD’s core symptoms. Harper et al. (2021) reported that integrating QbTest data with AI algorithms cut diagnostic uncertainty by 32% and reduced time to diagnosis by nearly three clinical visits on average.
2. Neuroimaging Applications
AI-driven analysis of structural and functional neuroimaging data is enabling the identification of ADHD-specific neural patterns. In a 2022 study, machine learning tools analyzing fMRI scans were able to diagnose ADHD with 85% accuracy by detecting atypical connectivity in executive function networks. This approach is particularly valuable for differentiating ADHD from other neurodevelopmental or psychiatric conditions with overlapping symptoms.
3. Virtual Reality Assessment Tools
Virtual reality (VR) platforms provide standardized, immersive environments replicating real-world scenarios more closely than traditional clinical assessments. Companies such as Akili Interactive have developed VR assessments that collect thousands of discrete behavioral data points per session. AI then analyzes this data for patterns consistent with ADHD while ensuring environmental consistency across tests, thereby minimizing confounding variables.
4. Digital Phenotyping
Smartphones and wearable technologies now passively collect behavioral data as individuals go about their daily routines. For instance, platforms like ADHD 360 evaluate smartphone use, physical activity, sleep patterns, and even social interactions to assemble a comprehensive behavioral profile. This method directly addresses the long-standing limitation of relying on in-clinic, artificial observations.
Collectively, the evolution of AI in assessment is not replacing clinical expertise. Instead, it is moving the field toward a balanced, integrated model where subjective impressions are augmented by robust, data-driven insights. This paradigm shift reframes ADHD as not only a cluster of behaviors, but as a condition characterized by distinct, measurable neurological and behavioral patterns.
Advantages of AI for ADHD Diagnosis
Enhanced Diagnostic Accuracy and Consistency
One of AI’s greatest advantages in ADHD assessment is improved diagnostic accuracy. A recent meta-analysis by Rossiter and Zhang (2021) covering 24 studies found that AI-augmented protocols achieved average sensitivity and specificity rates of 88% and 84%, compared to just 74% and 70% for standard clinical assessments.
Consistency across practitioners is another significant benefit. In a multi-site study across 12 clinical centers, the inter-rater reliability for traditional ADHD diagnosis was only 0.68, whereas AI-assisted systems reached an impressive 0.91. This enhanced consistency is particularly valuable for conditions like ADHD, where symptom expression can vary dramatically across different settings and times.
AI as a Clinical Decision Support Tool
AI is at its most powerful when used as a clinical decision support system, amplifying rather than overshadowing the clinician’s role. The Stanford ADHD Collaborative study revealed this synergy. Here’s what researchers observed:
- Clinicians working alone achieved 76% diagnostic accuracy.
- Standalone AI systems scored 83% accuracy.
- The combination of AI and clinician insights reached 92% accuracy.
AI rapidly processes vast, complex datasets to identify subtle behavioral or cognitive patterns. Clinicians then contextualize those findings within the patient’s personal history, existing conditions, and life context, marrying data-driven precision with human understanding.
Hybrid Diagnostic Models in Practice
The rise of hybrid models (melding AI and human expertise) has led to remarkable clinical improvements:
The FOCUS Protocol
Merging AI-analyzed behavioral data with structured clinical interviews, this approach reduced diagnostic uncertainty by 41% and led to 28% fewer unnecessary medication trials among a group of 450 children.
The NeuroTech Assessment Framework
Combining AI outputs from neuropsychological tasks, eye-tracking, and actigraphy with direct clinical observations, this framework, implemented in five pediatric centers, cut average diagnostic timelines from 18 months to just six weeks while upholding diagnostic accuracy.
Extending Assessment Beyond the Clinic
AI-powered tools are extending the reach of ADHD assessment to real-world environments. Here are two leading innovations:
Virtual Reality Ecological Assessment (VREA):
Creating lifelike simulations of classrooms or social situations, these platforms gather extensive behavioral data, providing a richer, more contextual view of symptoms. In one study, VREA platforms improved detection of situational ADHD symptoms by 31% compared to standard office-based methods.
Wearable Assessment Technologies:
Continuous Monitoring Platforms track activity, sleep, and physiological responses over days or weeks. This real-time, naturalistic approach has been particularly effective for adults whose ADHD symptoms may be less visible but functionally impactful. In a longitudinal study, wearable-based assessments identified 22% of adults with ADHD who had been missed by traditional diagnostic routes.
Capturing data in diverse settings and timeframes allows for a more complete picture of an individual’s functioning. It also supports identification of ADHD subtypes and individualized symptom patterns, aligning assessment with the movement toward personalized medicine. By precisely characterizing each person’s unique profile, care becomes truly tailored and actionable.
To further illustrate its diverse applications, similar AI-driven approaches are revolutionizing diagnostics and care in other sectors:
- Healthcare: AI assists in early detection of neurological disorders and chronic diseases, helping to close gaps in accessibility and reduce diagnostic delays.
- Education: Data-driven platforms personalize learning strategies by tracking attention, engagement, and progress, optimizing educational outcomes for students with diverse cognitive profiles.
- Workplace Management: Wearables and AI analytics support employee wellness, flagging patterns of stress or inattention for timely intervention.
Limitations and Challenges of ADHD Diagnosis AI
Data and Model Limitations
Despite major advances, AI-driven ADHD assessment tools are not without technical and ethical weaknesses. Most existing models have been trained on datasets that are overwhelmingly homogeneous. According to a review by Williams and Chen (2022), 78% of participants in ADHD AI training sets were male, and 67% were white, a sobering indicator of limited generalizability.
These training biases create performance disparities. For example, the NeuroDiverse Assessment Platform achieved 87% accuracy among participants reflecting its primary training demographic, but this dropped to just 64% for those from underrepresented backgrounds. Clearly, closing these demographic gaps is essential for fair and effective diagnosis.
Model transparency is another pressing issue. Many deep learning systems function as “black boxes,” making it difficult for clinicians or patients to understand how outcomes are determined. Such opacity is especially concerning when systems may misclassify or miss important contextual cues that human experts would catch.
Need for Diverse Training Datasets
Building truly representative AI models requires proactive efforts to include:
- Racial, ethnic, and cultural diversity
- Balanced gender representation
- All developmental stages, from early childhood to late adulthood
- Socioeconomic variety
- A spectrum of comorbid physical and mental health conditions
- Multiple cultural perspectives on symptom expression
Organizations like the International Neurodevelopmental AI Consortium have established minimum diversity thresholds for training sets (for example, capping any demographic at 40% of the total dataset). However, systemic barriers and historical inequities in research participation continue to make compliance difficult.
State of Clinical Validation
Rigorous, real-world clinical validation remains an ongoing challenge. Out of 17 commercial ADHD AI assessment tools reviewed by Martinez et al. (2023), only 5 had completed large-scale validation studies involving demographically diverse participants.
The transition from research prototype to clinical mainstay frequently exposes new challenges. AI models built on well-controlled data often struggle with complex, real-life cases—those involving multiple comorbidities, medication effects, and inconsistent environments. The FDA has responded by introducing the Digital Health Software Precertification Program, demanding continuous evaluation, transparency, and evidence of safety and efficacy before widespread adoption.
In addition, similar concerns arise in other fields relying on AI for critical decision-making:
- Finance: AI-based credit scoring must be continually monitored for bias and fairness to prevent unequal access.
- Healthcare: Predictive models used in diagnosis and treatment planning require ongoing validation to assure equitable healthcare outcomes.
- Legal: Automated document review and risk analysis tools must be designed to avoid reinforcing systemic biases.
Bridging the gap between promise and real-world reliability is central to responsible AI adoption in any sector.
Conclusion
The integration of artificial intelligence into ADHD assessment represents a genuine transformation. AI-powered tools supplement and sharpen clinicians’ abilities, improving accuracy, consistency, and ecological validity in a field long dominated by subjective impressions. This progress empowers both clinicians and neurodivergent individuals, shining a light on the uniquely dynamic nature of ADHD.
Yet, alongside these advancements, significant challenges persist. Gaps in representation, opaque model logic, and the lag in clinical validation demand that ethical standards and inclusivity rise in tandem with technological innovation.
For neurodivergent professionals, families, and their supporters, the promise is profound. When authentic lived experience and smart AI system design come together, AI can highlight strengths, foster adaptive systems, and promote genuine empowerment. Moving forward, the real opportunity lies not just in building more sophisticated algorithms, but in leveraging these tools to celebrate neurodiversity, eliminate bias, and advance truly individualized care.
As AI continues to evolve, those who center both human and machine intelligence will lead the way. They will reshape ADHD assessment into a process that is fair, actionable, and capable of adapting to every unique mind. The future will favor organizations and practitioners who combine data-driven innovation with an unwavering commitment to authenticity, equity, and person-centered support, redefining what it means for neurodivergent brilliance to thrive.




Leave a Reply